Unmasking Toxoplasmosis: How a Common Parasite Impacts Global Health, Behavior, and Future Disease Control. Discover the Hidden Dangers and Scientific Frontiers of Toxoplasma gondii. (2025)
- Introduction: What is Toxoplasmosis?
- Life Cycle and Transmission Pathways of Toxoplasma gondii
- Epidemiology: Global Prevalence and At-Risk Populations
- Clinical Manifestations: Symptoms in Humans and Animals
- Diagnosis: Current Methods and Emerging Technologies
- Treatment Options and Drug Resistance Challenges
- Toxoplasmosis in Pregnancy: Risks and Prevention
- Behavioral and Neurological Impacts: What the Research Shows
- Public Health Strategies and Prevention Initiatives (cdc.gov, who.int)
- Future Outlook: Vaccine Development, Public Awareness, and Projected 20% Increase in Research and Public Interest by 2030
- Sources & References
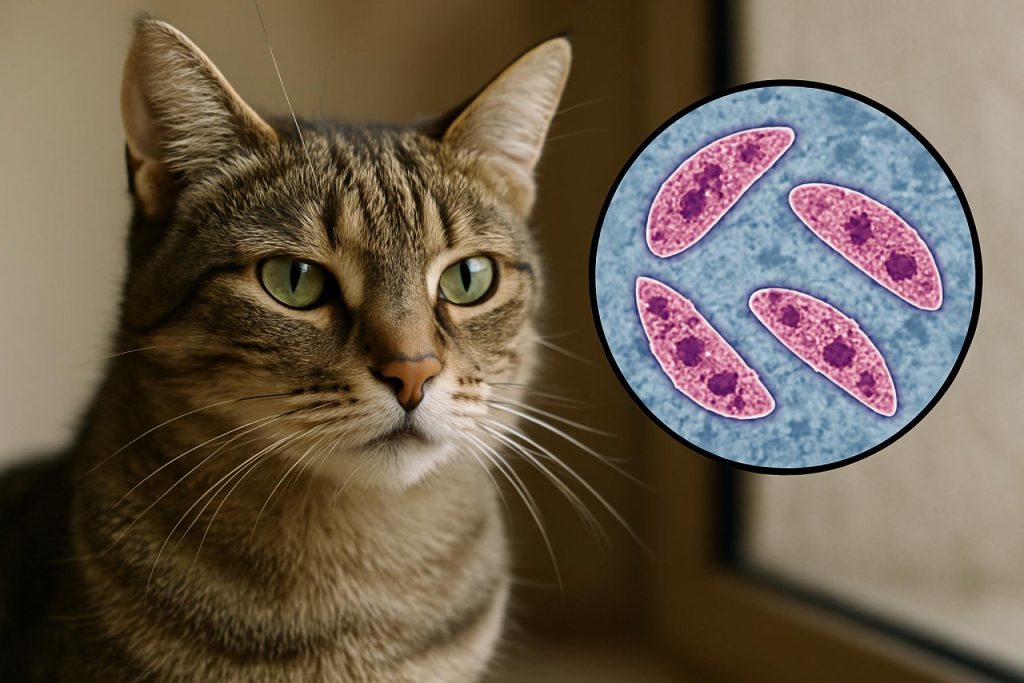
Introduction: What is Toxoplasmosis?
Toxoplasmosis is a parasitic infection caused by the protozoan Toxoplasma gondii. This organism is one of the most widespread parasites globally, capable of infecting virtually all warm-blooded animals, including humans. The primary host for T. gondii is the domestic cat and other felines, which play a crucial role in the parasite’s life cycle by shedding infectious oocysts in their feces. Humans and other animals typically become infected through ingestion of these oocysts from contaminated soil, water, or food, or by consuming undercooked meat containing tissue cysts. Less commonly, transmission can occur congenitally (from mother to fetus), via organ transplantation, or through blood transfusion.
Most healthy individuals infected with T. gondii experience mild or no symptoms, as the immune system usually keeps the parasite in check. However, toxoplasmosis can cause serious health problems in immunocompromised individuals, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or organ transplant recipients. In these populations, the infection can lead to severe neurological complications, ocular disease, or even death. Congenital toxoplasmosis, resulting from maternal infection during pregnancy, can cause miscarriage, stillbirth, or long-term neurological and ocular damage in the newborn.
Toxoplasmosis is recognized as a significant public health concern worldwide. According to the Centers for Disease Control and Prevention, it is one of the leading causes of foodborne illness-related deaths in the United States. The World Health Organization also highlights toxoplasmosis as a neglected parasitic disease, emphasizing the need for improved surveillance, prevention, and control strategies. The global prevalence of toxoplasmosis varies widely, influenced by factors such as dietary habits, climate, and the presence of cats in the environment.
Understanding toxoplasmosis is essential for both clinicians and the general public, given its potential impact on vulnerable populations and its often silent, yet persistent, nature. Ongoing research and public health initiatives aim to reduce the burden of this infection through education, improved diagnostic methods, and preventive measures.
Life Cycle and Transmission Pathways of Toxoplasma gondii
Toxoplasmosis is caused by the protozoan parasite Toxoplasma gondii, which exhibits a complex life cycle involving both definitive and intermediate hosts. The definitive hosts are members of the family Felidae (domestic and wild cats), where the parasite undergoes sexual reproduction. Intermediate hosts include a wide range of warm-blooded animals, including humans, in which only asexual reproduction occurs.
The life cycle of T. gondii begins when a cat ingests tissue cysts from infected prey. Within the feline intestine, the parasite undergoes sexual reproduction, resulting in the production of oocysts. These oocysts are shed in the cat’s feces and can contaminate soil, water, and food sources. Oocysts are highly resilient and can remain infectious in the environment for months. Intermediate hosts, such as rodents, birds, livestock, and humans, become infected primarily through ingestion of these sporulated oocysts from contaminated sources or by consuming undercooked meat containing tissue cysts.
Once ingested by an intermediate host, the oocysts release sporozoites that invade intestinal cells and differentiate into tachyzoites, the rapidly multiplying form responsible for acute infection. Tachyzoites disseminate throughout the body via the bloodstream, infecting various tissues. The host’s immune response eventually forces the parasite into a latent stage, forming bradyzoite-containing tissue cysts, particularly in neural and muscular tissues. These tissue cysts can persist for the lifetime of the host, and reactivation may occur if the host becomes immunocompromised.
Transmission pathways of T. gondii to humans are diverse. The most common routes include:
- Ingestion of food or water contaminated with oocysts from cat feces.
- Consumption of raw or undercooked meat containing tissue cysts, especially pork, lamb, or venison.
- Congenital transmission from an infected mother to her fetus, which can result in severe outcomes.
- Rarely, through organ transplantation or blood transfusion from an infected donor.
Environmental contamination is a significant concern, as oocysts can persist in soil and water, leading to outbreaks. Preventive measures focus on proper food handling, cooking meat thoroughly, and practicing good hygiene, especially for pregnant women and immunocompromised individuals. The global distribution and resilience of T. gondii oocysts underscore the importance of public health awareness and surveillance, as highlighted by organizations such as the Centers for Disease Control and Prevention and the World Health Organization.
Epidemiology: Global Prevalence and At-Risk Populations
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, is a globally distributed zoonotic infection with significant public health implications. The epidemiology of toxoplasmosis is complex, influenced by environmental, cultural, and socioeconomic factors. According to estimates, approximately one-third of the world’s human population has been exposed to T. gondii, though prevalence rates vary widely by region and population group.
The global seroprevalence of toxoplasmosis ranges from less than 10% in some countries to over 60% in others. Higher prevalence rates are typically observed in parts of Latin America, Central and Eastern Europe, the Middle East, and sub-Saharan Africa. In contrast, lower rates are reported in North America, Northern Europe, and Southeast Asia. These differences are attributed to variations in climate, dietary habits (such as consumption of undercooked meat), hygiene practices, and the presence of domestic cats, which are the definitive hosts of the parasite. The oocysts shed in cat feces can contaminate soil, water, and food, facilitating transmission to humans and other animals.
Certain populations are at increased risk for severe toxoplasmosis. Immunocompromised individuals, such as those with HIV/AIDS, organ transplant recipients, and patients undergoing chemotherapy, are particularly vulnerable to reactivation of latent infection, which can lead to life-threatening complications like encephalitis. Pregnant women represent another high-risk group; primary infection during pregnancy can result in congenital toxoplasmosis, potentially causing miscarriage, stillbirth, or severe neurological and ocular sequelae in the fetus. Infants born to mothers who acquire infection during gestation are at risk for long-term disabilities.
The World Health Organization (WHO) recognizes toxoplasmosis as a significant foodborne parasitic disease, emphasizing the need for improved surveillance and control measures. The World Health Organization and the Centers for Disease Control and Prevention (CDC) both provide guidance on prevention, diagnosis, and management of toxoplasmosis, highlighting the importance of public health education, especially for at-risk groups. Additionally, the World Organisation for Animal Health (WOAH, formerly OIE) monitors the disease in animals, given its zoonotic potential and impact on livestock.
In summary, toxoplasmosis remains a widespread infection with variable prevalence across the globe. Targeted interventions and awareness campaigns are essential to reduce transmission, particularly among vulnerable populations such as immunocompromised individuals and pregnant women.
Clinical Manifestations: Symptoms in Humans and Animals
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, presents with a wide spectrum of clinical manifestations in both humans and animals. The severity and nature of symptoms depend on the host’s immune status, age, and whether the infection is acute or chronic.
In immunocompetent humans, toxoplasmosis is often asymptomatic or manifests as mild, self-limiting symptoms. When present, these may include low-grade fever, lymphadenopathy (especially cervical), muscle aches, and fatigue. Some individuals may experience flu-like symptoms, which can be mistaken for other viral infections. Ocular toxoplasmosis, a more severe form, can occur when the parasite invades the retina, leading to blurred vision, eye pain, and in some cases, permanent vision loss. This is a significant cause of posterior uveitis worldwide (Centers for Disease Control and Prevention).
In immunocompromised individuals, such as those with HIV/AIDS, organ transplant recipients, or patients undergoing chemotherapy, toxoplasmosis can reactivate from latent tissue cysts. This reactivation often leads to severe manifestations, including encephalitis, characterized by headache, confusion, seizures, and focal neurological deficits. Disseminated disease may also involve the lungs, heart, and other organs, and can be life-threatening without prompt treatment (World Health Organization).
Congenital toxoplasmosis occurs when a woman acquires primary infection during pregnancy and transmits the parasite to the fetus. The risk and severity of fetal infection depend on the gestational age at the time of maternal infection. Early infection can result in miscarriage, stillbirth, or severe neurological and ocular damage in the newborn, including hydrocephalus, intracranial calcifications, and chorioretinitis. Later infections may be less severe but can still cause long-term sequelae (Centers for Disease Control and Prevention).
In animals, clinical manifestations vary by species. Cats, the definitive hosts, are usually asymptomatic but can occasionally develop mild diarrhea, pneumonia, or ocular lesions. In livestock such as sheep and goats, toxoplasmosis is a leading cause of abortion and neonatal mortality. In dogs and other mammals, symptoms may include fever, lethargy, respiratory distress, and neurological signs. The disease’s impact on animal health has significant economic implications, particularly in the livestock industry (World Organisation for Animal Health).
Overall, the clinical spectrum of toxoplasmosis is broad, ranging from asymptomatic infection to severe, life-threatening disease, underscoring the importance of awareness and early diagnosis in both human and veterinary medicine.
Diagnosis: Current Methods and Emerging Technologies
Diagnosis of toxoplasmosis, an infection caused by the protozoan parasite Toxoplasma gondii, is critical for effective patient management, especially in immunocompromised individuals, pregnant women, and neonates. The diagnostic landscape encompasses serological, molecular, and imaging techniques, with ongoing advancements aimed at improving sensitivity, specificity, and rapidity.
Serological Methods remain the cornerstone of toxoplasmosis diagnosis. Detection of specific immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies against T. gondii in serum is widely used to distinguish between acute and chronic infections. Enzyme-linked immunosorbent assays (ELISA), immunofluorescence assays (IFA), and the Sabin-Feldman dye test are among the most established techniques. The Centers for Disease Control and Prevention (CDC) recommends serological testing as the first-line approach, with IgM positivity suggesting recent infection and IgG indicating past exposure. However, false positives and persistent IgM can complicate interpretation, necessitating confirmatory testing or avidity assays to assess the timing of infection.
Molecular Diagnostics have gained prominence, particularly polymerase chain reaction (PCR)-based assays, which detect T. gondii DNA in blood, cerebrospinal fluid, amniotic fluid, or tissue samples. PCR is especially valuable in congenital toxoplasmosis, immunocompromised patients, and cases with ambiguous serology. The World Health Organization (WHO) recognizes PCR as a highly sensitive and specific tool, though its availability may be limited in resource-constrained settings. Quantitative PCR (qPCR) further enables parasite load estimation, aiding in disease monitoring and prognosis.
Emerging Technologies are shaping the future of toxoplasmosis diagnostics. Point-of-care (POC) tests, such as rapid immunochromatographic assays, are being developed to facilitate timely diagnosis in low-resource environments. Advances in biosensor technology, microfluidics, and next-generation sequencing (NGS) hold promise for multiplexed, high-throughput detection of T. gondii and differentiation from other pathogens. Research into novel biomarkers, including circulating antigens and microRNAs, is ongoing to enhance early detection and disease staging.
Imaging Modalities such as magnetic resonance imaging (MRI) and computed tomography (CT) are adjunctive tools, particularly in diagnosing cerebral toxoplasmosis in immunocompromised patients. These modalities help identify characteristic brain lesions but are not specific to T. gondii infection and must be interpreted alongside laboratory findings.
In summary, the diagnosis of toxoplasmosis in 2025 relies on a combination of serological and molecular methods, with emerging technologies poised to improve accessibility, accuracy, and speed. Continued collaboration among global health authorities, such as the Centers for Disease Control and Prevention and the World Health Organization, is essential to standardize and disseminate best practices in toxoplasmosis diagnostics.
Treatment Options and Drug Resistance Challenges
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, presents significant therapeutic challenges, particularly in immunocompromised individuals and pregnant women. The standard treatment for acute toxoplasmosis typically involves a combination of pyrimethamine and sulfadiazine, administered alongside folinic acid to mitigate hematologic toxicity. This regimen targets the parasite’s folic acid synthesis pathway, effectively inhibiting its replication. In cases where sulfadiazine is contraindicated due to allergy or intolerance, clindamycin is often substituted. For less severe or ocular cases, trimethoprim-sulfamethoxazole may be considered as an alternative therapy. Despite these options, treatment is not always curative, as the drugs primarily target the tachyzoite stage and have limited efficacy against tissue cysts (bradyzoites), which can persist in the host and reactivate under immunosuppression.
Drug resistance in T. gondii is an emerging concern, though it is less prevalent compared to other protozoan infections. Resistance mechanisms are not fully understood but may involve mutations in the dihydrofolate reductase-thymidylate synthase gene, reducing the efficacy of pyrimethamine and related agents. Additionally, the parasite’s ability to form latent tissue cysts contributes to therapeutic challenges, as current medications do not eradicate these forms. This persistence underlines the need for novel therapeutics capable of targeting both active and latent stages of the parasite.
For immunocompromised patients, such as those with HIV/AIDS or organ transplant recipients, long-term maintenance therapy is often required to prevent reactivation. The Centers for Disease Control and Prevention (CDC) recommends ongoing prophylaxis with agents like trimethoprim-sulfamethoxazole in high-risk populations. Pregnant women with acute infection are managed with spiramycin, particularly in the first trimester, to reduce the risk of congenital transmission, as recommended by the World Health Organization (WHO). However, spiramycin is not universally available, and its efficacy in preventing fetal infection is variable.
Research into new treatment modalities is ongoing, with efforts focused on developing drugs that can penetrate tissue cysts and overcome resistance mechanisms. Immunotherapy and vaccine development are also areas of active investigation, aiming to provide long-term protection and reduce the global burden of toxoplasmosis. The complexity of the parasite’s life cycle and its ability to evade host immunity continue to pose significant obstacles to effective management and eradication.
Toxoplasmosis in Pregnancy: Risks and Prevention
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, poses significant health risks during pregnancy. While infection is often asymptomatic in healthy adults, primary infection acquired during pregnancy can result in severe consequences for the developing fetus. The parasite is commonly transmitted through ingestion of undercooked contaminated meat, exposure to oocysts from cat feces, or consumption of contaminated water or soil. Vertical transmission from mother to fetus is the primary concern in pregnancy, as it can lead to congenital toxoplasmosis.
The risk of fetal infection depends on the gestational age at which the mother acquires the infection. Transmission rates increase with advancing gestation, but the severity of fetal disease is greatest when infection occurs in the first trimester. Congenital toxoplasmosis can result in miscarriage, stillbirth, or a range of severe outcomes in the newborn, including hydrocephalus, chorioretinitis, intracranial calcifications, and long-term neurological deficits. Some infants may appear healthy at birth but develop symptoms later in life.
Prevention of toxoplasmosis in pregnancy relies on education and behavioral modifications. Pregnant individuals are advised to avoid consumption of raw or undercooked meat, thoroughly wash fruits and vegetables, and practice good hand hygiene, especially after handling raw meat or soil. Contact with cat litter should be minimized, and if unavoidable, gloves should be worn and hands washed thoroughly afterward. Cats, the definitive hosts of T. gondii, should be fed only commercial or well-cooked food and kept indoors to reduce their risk of infection.
Routine serological screening for toxoplasmosis during pregnancy is not universally implemented, but some countries with higher prevalence rates have adopted such programs. Early detection of maternal infection allows for prompt intervention, including antiparasitic therapy, which may reduce the risk and severity of fetal infection. The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) provide guidelines on prevention, diagnosis, and management of toxoplasmosis in pregnancy. These organizations emphasize the importance of public health education and targeted screening in high-risk populations.
- Primary prevention: Avoid undercooked meat, unwashed produce, and contact with cat feces.
- Secondary prevention: Early detection and treatment of maternal infection to reduce fetal risk.
- Public health: Education campaigns and, where appropriate, routine screening in pregnancy.
In summary, toxoplasmosis remains a preventable cause of congenital infection. Adherence to preventive measures and, where indicated, screening and treatment protocols are essential to protect maternal and fetal health.
Behavioral and Neurological Impacts: What the Research Shows
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, is widely recognized for its potential to affect the central nervous system, leading to a range of behavioral and neurological impacts in both humans and animals. Research over the past decades has increasingly focused on the subtle, long-term effects of chronic or latent infection, particularly in immunocompetent individuals who may not exhibit acute symptoms.
One of the most compelling areas of study involves the association between latent toxoplasmosis and behavioral changes. Animal models, especially rodents, have demonstrated that infection with T. gondii can alter innate behaviors—such as reducing aversion to predator odors—which is hypothesized to facilitate the parasite’s life cycle by increasing the likelihood of transmission to feline hosts. These findings have prompted investigations into whether similar behavioral modifications occur in humans. Epidemiological studies suggest a correlation between latent toxoplasmosis and increased risk-taking, altered reaction times, and even changes in personality traits. Some research has also linked infection to a higher incidence of traffic accidents and risk-prone behaviors, though causality remains under debate.
Neurologically, T. gondii has a predilection for neural tissue, where it can form cysts and persist for the host’s lifetime. In immunocompromised individuals, such as those with HIV/AIDS, reactivation of the parasite can lead to toxoplasmic encephalitis, a severe and potentially fatal condition characterized by confusion, seizures, and focal neurological deficits. In the general population, chronic infection has been associated with subtle neurocognitive effects, including mild memory impairment and slower psychomotor performance. There is also ongoing research into the possible link between toxoplasmosis and psychiatric disorders, such as schizophrenia and bipolar disorder. While some studies have reported a higher prevalence of T. gondii antibodies in individuals with these conditions, the mechanisms underlying this association are not fully understood and remain an active area of investigation.
Major health organizations, including the Centers for Disease Control and Prevention and the World Health Organization, recognize the neurological risks posed by toxoplasmosis, particularly for vulnerable populations. They emphasize the importance of preventive measures, early diagnosis, and appropriate treatment to mitigate the potential long-term impacts of infection. As research continues, a clearer understanding of the behavioral and neurological consequences of toxoplasmosis will inform public health strategies and clinical management.
Public Health Strategies and Prevention Initiatives (cdc.gov, who.int)
Toxoplasmosis, caused by the protozoan parasite Toxoplasma gondii, remains a significant public health concern worldwide due to its potential to cause severe disease in immunocompromised individuals and congenital infections in newborns. Public health strategies and prevention initiatives are essential to reduce the incidence and impact of toxoplasmosis, particularly among vulnerable populations such as pregnant women and individuals with weakened immune systems.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) are leading authorities in the development and dissemination of guidelines for toxoplasmosis prevention. Both organizations emphasize the importance of public education campaigns to raise awareness about the routes of transmission, which include ingestion of undercooked or raw meat containing tissue cysts, exposure to oocysts from contaminated soil or water, and contact with cat feces.
Key public health strategies recommended by these organizations include:
- Food Safety: Promoting the thorough cooking of meat, washing fruits and vegetables, and avoiding unpasteurized dairy products to minimize the risk of ingesting infectious forms of the parasite.
- Hygiene Practices: Encouraging regular handwashing, especially after handling raw meat, soil, or cat litter, and using gloves when gardening or cleaning litter boxes.
- Pregnancy Precautions: Advising pregnant women to avoid changing cat litter if possible, or to use gloves and wash hands thoroughly afterward, and to undergo serological screening in high-risk areas to identify and manage acute infections early.
- Veterinary and Animal Control Measures: Recommending that domestic cats be fed commercial or well-cooked food and kept indoors to reduce their exposure to the parasite, thereby limiting environmental contamination.
- Water Safety: Supporting initiatives to improve water sanitation and prevent contamination with oocysts, particularly in regions where waterborne outbreaks have occurred.
The CDC also collaborates with state and local health departments to monitor toxoplasmosis cases and outbreaks, providing technical assistance and surveillance data to inform targeted interventions. The WHO integrates toxoplasmosis prevention into broader maternal and child health programs, especially in endemic regions, and supports research into vaccine development and improved diagnostic tools.
Ongoing public health efforts focus on reducing the burden of toxoplasmosis through a combination of education, surveillance, and evidence-based interventions, with the goal of protecting at-risk populations and minimizing the global impact of this parasitic disease.
Future Outlook: Vaccine Development, Public Awareness, and Projected 20% Increase in Research and Public Interest by 2030
The future outlook for toxoplasmosis management and prevention is shaped by ongoing advances in vaccine development, increasing public awareness initiatives, and a projected surge in research and public interest. As of 2025, toxoplasmosis remains a significant global health concern, particularly for immunocompromised individuals and pregnant women. The causative agent, Toxoplasma gondii, is a protozoan parasite with a complex life cycle, making vaccine development challenging. However, recent years have seen promising progress in both veterinary and human vaccine research. Several candidate vaccines targeting different stages of the parasite’s life cycle are under investigation, with some showing efficacy in animal models. The development of an effective human vaccine remains a high priority, as it could dramatically reduce congenital infections and disease burden in vulnerable populations. Leading organizations such as the World Health Organization and the Centers for Disease Control and Prevention continue to monitor and support research in this area.
Public awareness campaigns are also expected to expand significantly by 2030. These initiatives focus on educating at-risk groups about preventive measures, such as proper food handling, avoiding consumption of undercooked meat, and practicing good hygiene when handling cat litter. Enhanced awareness is crucial for reducing transmission rates, especially in regions with high seroprevalence. National and international health agencies are increasingly collaborating to disseminate accurate information and resources, leveraging digital platforms and community outreach programs.
Looking ahead, a projected 20% increase in research activity and public interest in toxoplasmosis is anticipated by 2030. This growth is driven by heightened recognition of the disease’s impact on public health, its potential links to neuropsychiatric disorders, and the need for improved diagnostic and therapeutic tools. Funding agencies and research institutions are expected to allocate greater resources to basic and translational research, fostering innovation in diagnostics, treatment, and prevention strategies. The anticipated rise in public engagement is likely to further stimulate policy development and resource allocation, creating a positive feedback loop that accelerates progress in the field.
- Vaccine development is advancing, with several promising candidates in preclinical and early clinical stages.
- Public awareness campaigns are expanding, targeting both general and high-risk populations.
- Research and public interest in toxoplasmosis are projected to increase by 20% by 2030, driving innovation and policy support.
Continued collaboration among international health organizations, research institutions, and public health agencies will be essential to realize these advancements and reduce the global burden of toxoplasmosis in the coming decade.



